Dr. James Clarkson, Chief Medical Officer of WAVR Inc., is a skilled plastic and hand surgeon focused on revolutionizing local anesthetic surgeries through “Wide Awake Virtual Reality” (WAVR). This technology reduces anxiety, lowers costs, improves workflow, and enhances patient education by shifting surgeries from hospitals to offices. Alongside his role at WAVR, Clarkson is an Assistant Professor at Michigan State University College of Human Medicine. His career, including 12 years with the British NHS, is marked by innovation and a strong commitment to the doctor-patient relationship.
Chief Medical Officer of WAVR Inc.
Doctor James Clarkson, current Chief Medical Officer of WAVR Inc., is an accomplished plastic and hand surgeon, educator, and executive seeking to change the way patients experience localized surgeries by utilizing “Wide Awake Virtual Reality”, or WAVR. WAVR is proven to enhance the patient experience by reducing anxiety, increasing joy, and overall simplifying the complex process of surgical anesthetics that have become commonplace in healthcare today. Through his personal experience utilizing WAVR in surgical settings, Clarkson campaigns that Virtual Reality decreases costs, improves workflow, and increases productivity by taking localized surgeries out of the hospital and back into the office, benefiting both patients and physicians alike. He also demonstrates that VR can provide a more convenient and sticky educational experience for patients, helping them understand their surgery and post-operative instructions.
Assistant Professor of Surgery, MSU
In addition to serving as the CMO at WAVR Inc., Clarkson works as an Assistant Professor of Surgery and a practicing Hand Surgeon at Michigan State University..
,. Clarkson has conducted studies for the last six years as he has utilized Virtual Reality in his surgeries, which trial data and outcomes further prove the efficacy of this technology to revolutionize the standard of care for patients.
International background
Dr Clarkson trained as a Plastic Surgeon in the British National Health, qualifying from the London Hospital Medical School in 1995 and completing his specialty training in Plastic Surgery in 2008. Clarkson served as a physician for a twelve-year tenure in the British National Health Service before his emigration to the United States, bringing with him the knowledge and expertise he gained working in the world’s largest socialized healthcare system. The throughline of Clarkson’s career is that of a commitment to healthcare justice, innovation, decomplexification and placing the Doctor-Patient relationship at the pinnacle of the surgical process.
Fellowship training, Boards and Medical Societies
He is double board certified in Plastic Surgery from the Royal College of Surgeons Edinburgh (2007) and the Royal College of Physicians and Surgeons of Canada, (2014)
He spent 2 years at the Christine Kleinert Institute of Hand and Microsurgery between 2008 and 2010.
He is a member of the American Society of Plastic surgeons and sits on their Patient Safety and Healthcare Delivery Subcommittees.

The development of VR to enable office based WALANT surgery: A surgeons journey.
In 2016, I seized the opportunity to redirect my Plastic Surgery practice at Michigan State University from Head and Neck Microvascular Reconstruction, back to my passion for Hand Surgery. My goal was to simplify patient care, thereby reducing unnecessary risks and costs while enhancing the overall patient experience. Inspired by Dr. Don Lalonde’s advocacy for WALANT (Wide Awake Local Anesthesia No Tourniquet) surgery, I began to offer awake hand surgery in an office setting.
However, many of my patients were used to the option of sedation, and initially, about a third of them were hesitant to undergo surgery without it. One evening, while playing with my sons, aged 6 and 8, using a new Galaxy VR headset for my phone, I observed how deeply engrossed they became in the virtual reality environment. This observation sparked an idea about the potential of VR to distract patients during surgery.
I quickly implemented VR as an option for my patients, starting with a patient who had an anxiety disorder in December 2016. The response was overwhelmingly positive. With VR, I could now offer a middle ground between fully awake surgery and sedation, telling my patients, “I won’t put you out, but I can put you somewhere else.” I added education content to prepare my patients for recovery. After introducing VR, no one declined the option of having their surgery in the office. This innovation not only improved patient comfort but also streamlined the surgical process, making office-based hand surgery more accessible and less daunting for everyone involved, including the surgical team.
I won’t put you out but I can put you somewhere else

2016, The first use of VR to enable office based WALANT hand surgery
In 2019 I presented the results of a blinded trial into the use of VR during awake hand surgery, finding that it reduced anxiety and increased enjoyment for my patients. For those patients who already had an anxiety disorder we also saw a reduction in the pain of local anesthetic injection from 5.5/10 to 2.5/10. Those without anxiety disorder reported 2.5, so VR had normalized the experience for my anxiety sufferers.
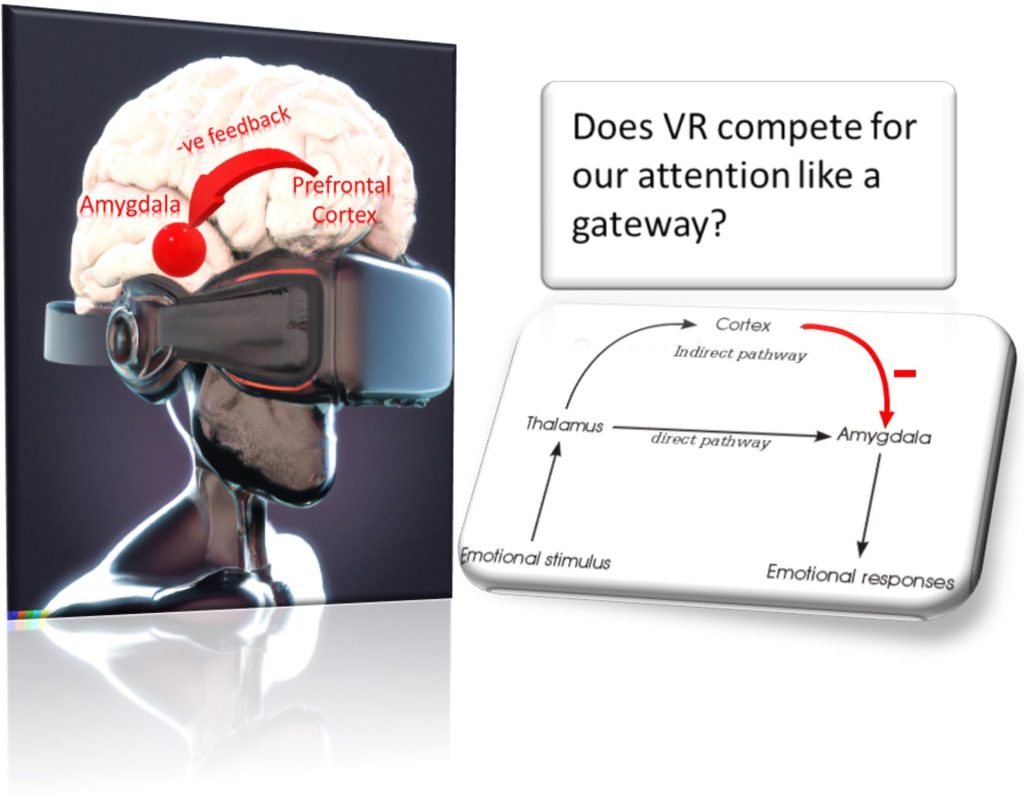
I went on to publish studies into larger numbers of patients, the effect of the office on infection rates and the patient experience and the use of VR in wound care. From these studies I was able to hypothesis that VR worked through the cortex to re-contextualize our experience of fear and anxiety.
I have performed over 3000 hand operations using VR in the office setting since 2016.

Family Life:
Dr Clarkson lives with his family in Okemos, Michigan and enjoys his weekends in Benzie County Michigan on the Betsie river teaching his growing boys his love of nature.

